CPER Digest
ISSUE 11
You respond on a low priority for a 68 year old female patient who has slipped down the last two steps while coming out of a local church. She suffered no LOC, did not strike her head at all, and the fall was witnesses by family menbers. They state it appears as if she rolled her ankle on the last step and there is some obvious swelling to the L ankle, with good CSM and a pedal pulse intact. She remains conscious and alert, however is unable to weight bear at this time due to the pain. She states it is severe 8/10 pain that is "sharp and throbbing."
Physical exam/General Appearance - Seated on the bottom step of the staircase. No other obvious trauma is noted on a rapid trauma exam. She is slightly sweaty but otherwise good colour. She is holding her L ankle which is obviously swollen and has some mild discolouration/bruising. Deformity is difficult to ascertain due to such however skin is not broken. She states she tried to get up once but sat back down because of the pain.
- Medical history: Hypertension, hypercholesterolemia, hypothyroid. No previous surgeries.
- Current medications: Amlodipine, clopidogrel, levothyroxine
- Allergies: None Under the Analgesia Medical Directive what medications can this patient receive for her pain, if any?
Under the Analgesia Medical Directive what medications can this patient receive for her pain, if any?
Answer
This patient qualifies for any pain option for both the PCP and ACP scope.
Remember that clopidogrel is not an anticoagulant but an antiplatelet agent and this patient can still receive ibuprofen or ketorolac.
Excluding NSAIDs in this case would be an unnecessary omission that still persists despite frequent education, given confusion about anticoagulants and antiplatelets.
Analgesia tips and tricks:
- Slow. Down. While appreciably as clinicians we want to treat patients pain and discomfort as soon as we can, analgesia is not something that needs to be rushed. Take the time to go through the patients medication list and look carefully for anticoagulants before administering. We've attached a list of common medications below.
- Medical history can also clue you in to the possibility of anticoagulants before you even seethe medication list. Common conditions that trigger anticoagulation include A-fib, CVA, artificial heart valves, pacemaker, and DVT/PE. Obviously this is not a guarantee but may help guide your information gathering.
- Generally speaking stick with one route. If the patient qualifies for PO meds, then administer acetaminophen and ibuprofen. Note that ketorolac is not "better" or more effective, it should be used if oral route is not an option (i.e. significant vomiting in possible renal colic or migraine pattern headaches).
- Remember to reduce your acetaminophen dose for ages 12-17.
- Don't try to remember all contraindications. We are human and this can lead to error. Use your directive books/app each time to confirm. This allows you to go through the questionswith the patient directly and it may also refresh their memory on something they're forgetting.
ACPs:
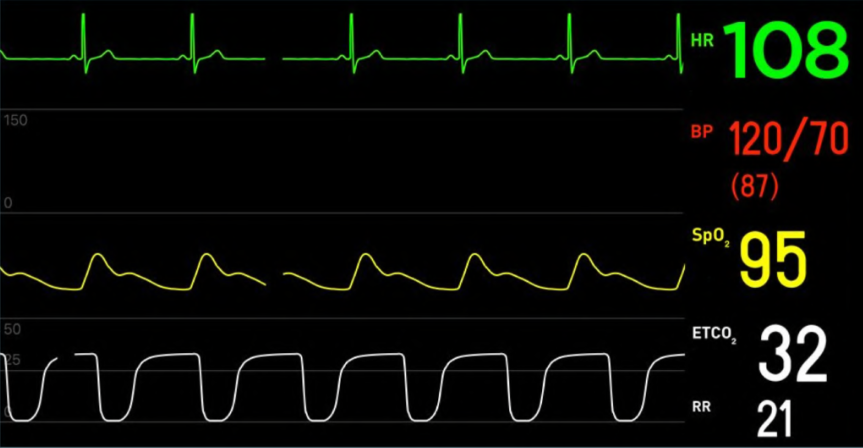
A question we receive occasionally is if the patient is hypotensive but becomes normotensive can opioids be administered? The short answer is yes. The long answer is carefully consider what you think the underlying cause of hypotension is. For example if it's an elderly patient that fell due to weakness because they have had little intake and you correct with some fluid, this would be relatively safe. If it's due to possible GI hemorrhage or multiple medications it may need more careful consideration, smaller doses or an OMC consultation.
| Common Anticoagulants (NSAIDs contraindicated) |
Common antiplatelet (OK for NSAIDs) |
|---|---|
| Warfarin (Coumadin) Apixaban (Eliquis) Dabigatran (Pradaxa) Rivaroxaban (Xarelto) |
Acetylsalicylic Acid / ASA (Aspirin, Entrophen) Clopidogrel (Plavix) Ticagrelor (Brilinta) |
Watch Dr. Miller's IG reel on anticoagulants / antiplatelets